Foot and ankle surgery is a specialised area of orthopaedic surgery. The surgery can be quite challenging and every patient is different with unique needs and goals.
You will need to follow instructions, perform appropriate exercises, and modify your activities during your healing process.
This requires patience, persistence, and a desire to get better. If you are unable to complete the post-operative instructions it will affect your results and you should consider alternative treatments.
Successful results from surgery require a contribution from you.
Whenever surgery is considered we always try to minimise the risks. You are already on this path by consulting an experienced orthopaedic surgeon who is a specialist in foot and ankle disorders. The body is a very complex and varied structure so although we aim for perfection, no specialist can give perfect results every time.
It is important that you read all of the information carefully. The information provided is intended to be a guide and not all-inclusive. If you have any questions, concerns, or are not certain about the benefits, risks, limitations, or alternatives to your treatment, please do not hesitate to ask your surgeon.
PREPARING FOR SURGERY
- On the morning of surgery please shower and thoroughly wash your feet and toes with soap (anti-bacterial if available) and water.
- Fast from the time instructed.
- On the day of surgery do NOT take any Insulin or diabetes tablets unless otherwise instructed. (If you are normally on Insulin please confirm with us that we have this information). Aspirin and any blood thinners (e.g. warfarin, Plavix, Iscover) should have been stopped one week before surgery.
- Otherwise please take your normal medications (e.g., blood pressure tablets) with a small sip of water.
- Attend hospital at appropriate time – there may be some waiting time before your surgery but you need to arrive so that you can be checked in by the nursing staff and seen by the anaesthetist beforehand. Please bring a book, magazine or music in case of a moderate wait or delay.
- Remember to bring your X-rays / Scans please.
PAIN MANAGEMENT
A local anaesthetic block may be given to you during surgery. This will produce numbness around the nerves in the region of your surgical procedure. It will provide you with pain relief for approximately 12-18 hours post-operatively, enabling you to be comfortable and allow sleep after your surgery. It will also allow time to take some of your oral painkillers prior to the block wearing off and prevent a sudden onset of pain.
It is best to take your painkillers regularly for the first 1-2 weeks. Initially, prescription medication is usually necessary and after the initial 2-3 days, regular Panadol or Panadeine is usually all that is required.
It is also worthwhile taking painkillers prior to your first post-operative visit to ensure that plaster and suture removal is more comfortable.
Remember, pain is better managed if you get on top of it before it gets on top of you.
DRESSINGS AND EXTERNAL PINS
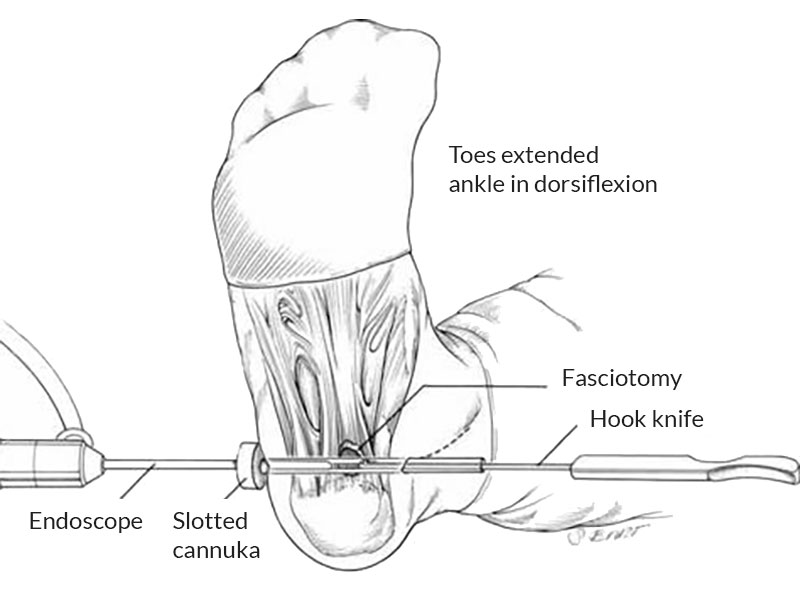
- Please leave your bandages intact until reviewed by your surgeon at the postoperative visit (except for ankle scopes and plantar fascia release where the outer bandage can be removed after 2 days). A plastic garbage/kitchen bag sealed with tape and elastic band +-‘glad wrap’ is needed to keep it dry in the shower or bath. If there is excessive bleeding leaking through the bandage or the bandages get wet please contact the rooms and this can easily be re-bandaged if required.
- Rest and elevation of your foot (to at least the level of your hip and ideally above the level of your heart) is required for the first 10 days following surgery. This helps minimise swelling and aids healing of your wounds.
- Icing of the area (if possible) for 20 minutes 2-3 times per day for the first 3-5 days can also help reduce swelling and pain.
- If part of your wound continues to ooze, this usually only requires regular dressing changes. If you have any concerns, please contact the rooms prior to commencing any antibiotics.
- Similarly, if the pins used to straighten your toes are knocked, it is unusual to do any damage. However if the toe becomes deformed or there is prolonged pain then contact the rooms.
- Gentle leg, ankle, foot and toe movement and stretching (if possible and not in plaster) every hour will help with circulation and muscle recovery.
- If you have been instructed to be ‘non-weight bearing’ this is to allow best healing of bones/tendons/ligaments.Failure to comply may jeopardise the results of your surgery.
- Time off work and recovery will depend on the nature of your surgery. Generally a minimum of one to two weeks is required off for seated/ deskwork (unless very minor surgery). For more prolonged standing or walking this will often require at least 4-6 weeks (or longer).
- A ’post-op’ appointment will be made 2 weeks after surgery for removal of stitches and to check the healing of your wounds. The next follow up will usually be a further 4-6 weeks later to check further recovery.
- If physiotherapy is required this will be arranged/ discussed at your follow up appointment.
SWELLING
Swelling often increases over the first 6 weeks and then usually reduces over the next 6 weeks. Depending on the nature and magnitude of the surgery, it may take up to 12 months to fully settle. This is the normal way the body heals. Rest and elevation is helpful. As the foot swells it is common to have stiffness and mild nerve pain so attention to swelling is important.
EXERCISE
However, do not overdo it. Too much too early can be just as bad as not doing enough. This includes sport. Your surgeon is happy to liaise with your trainers to get you back on the field as quickly as possible without compromising your recovery process and long-term health.
COMPLICATIONS
Fortunately complications are uncommon. Nevertheless they do occur and you need to be aware of them. The following is a non-exhaustive list of some of the more frequent. You should also be aware that several factors can increase your chance of having a complication. These include smoking, diabetes, and obesity. You can reduce this risk by quitting smoking, good blood sugar control, and losing weight.
INFECTION
This occurs when the wound is invaded by bacteria, usually from your surrounding skin. Signs you may have an infection include heat, tenderness, unusual fluid, or an odour coming from your wound. You may also have a fever or feel generally unwell. Most infections can be treated with antibiotics but more serious ones require admission to hospital and further surgery to clean out the wound.
WOUND HEALING
Normal wound healing requires adequate blood flow and active healing cells. Being too active early after surgery causes bleeding and swelling which can cause part of the wound to open. The foot is very delicate in this respect. It is important that you rest and keep your foot elevated as much as possible for the first 7-10 days to encourage healing and discourage wound break down. Risks of infection and healing problems are much higher if you smoke or are diabetic. If you are able to give up smoking before and for a few weeks after your surgery this will help your healing process.
NERVES
Nerves are the electrical system of the body. It is extremely rare for nerves to be cut but nerves are commonly affected by swelling after surgery. This can cause partial numbness and sometimes burning pain. This generally resolves as the swelling subsides. In rare cases this can persist.
STIFFNESS
Both injury and surgery create scar tissue. Some people are prone to develop excess scar tissue. When this is combined with post-operative swelling it may lead to joint stiffness. Most of this can be addressed through good quality rehabilitation techniques and your own involvement in recovery.
BONE HEALING
Surgeons can only create the environment for bone healing. It is your body that performs the final joining process. This can fail if there is too much mobility (i.e. you walk on it too early) or if there are other issues such as smoking, blood flow problems or infection. If the bone fails to heal it may require further surgery.
DEEP VEIN THROMBOSIS (DVT) AND PULMONARY EMBOLISM (PE)
These fortunately are very rare events but can have serious consequences. Signs you may have a DVT include swelling that is not reduced with elevation of the leg, colour changes or coldness of the toes, calf pain or tenderness. Signs you may have a PE include chest pain or shortness of breath. Seek immediate medical attention if you are concerned.
PROLONGED OR EXCESSIVE PAIN
This can be a sign of a variety of complications following surgery, with many mentioned previously. On very rare occasions a chronic regional pain syndrome can develop in addition to these and require further prolonged management.
ANAESTHETIC (GENERAL, SPINAL, NERVE BLOCKS)
Any concerns should be discussed with your anaesthetist during the pre-operative consultation.
After surgery you should notify your surgeon / GP / Emergency department if you have any of the following:
- Increasing pain (despite painkillers, rest elevation and icing).
- Increasing swelling (despite rest and elevation above the level of your heart).
- Fevers or sweats.
- Discharge or increasing redness of your wound.
- Shortness of breath or chest pains.
- Persistent numbness (greater than 48hrs after surgery).
For most surgeries it takes a minimum of 3 months to be recovering reasonably well (75%), 6 months until 90% recovered and 12 months until complete recovery. Swelling is normal for the first 3-4 months and can take 6-12 months before full recovery is expected.
Note: These notes have been prepared by orthopaedic surgeons.They are general overviews and information aimed for use by their specific patients and reflects their views, opinions and recommendations. This does not constitute medical advice. The contents are provided for information and education purposes only and not for the purpose of rendering medical advice. Please seek the advice of your specific surgeon or other health care provider with any questions regarding medical conditions and treatment.